Clinical Evidence
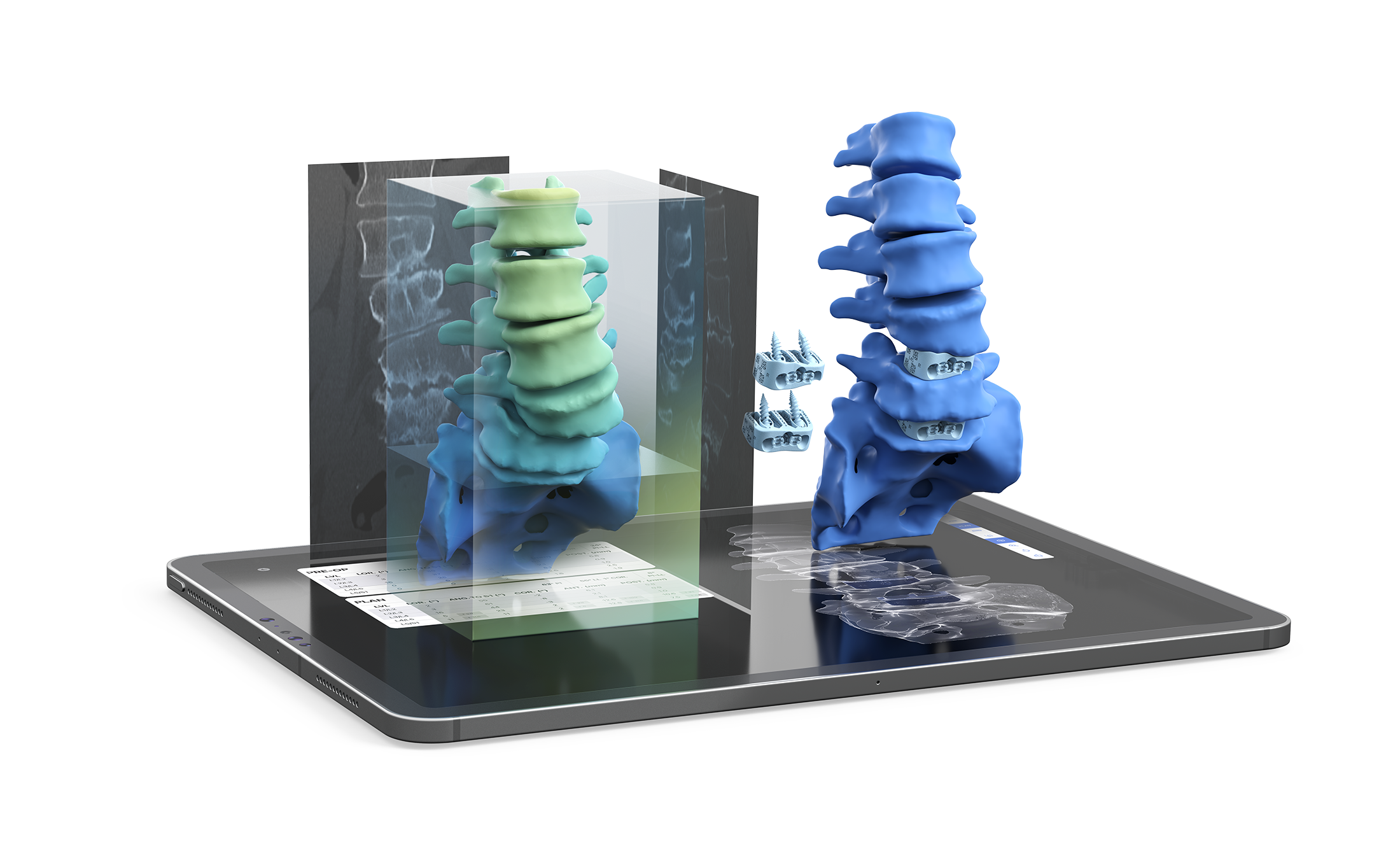
Clinical evidence is essential, and we understand that evidence of superior clinical performance is paramount to delivering exceptional patient care. Published data on over 500 patients shows that aprevo® improves surgical outcomes against the standard of care in both degenerative lumbar disease and adult spinal deformity.
Predictable Intervertebral Alignment:
82% of personalized aprevo® interbody levels achieved targeted alignment within 5°1
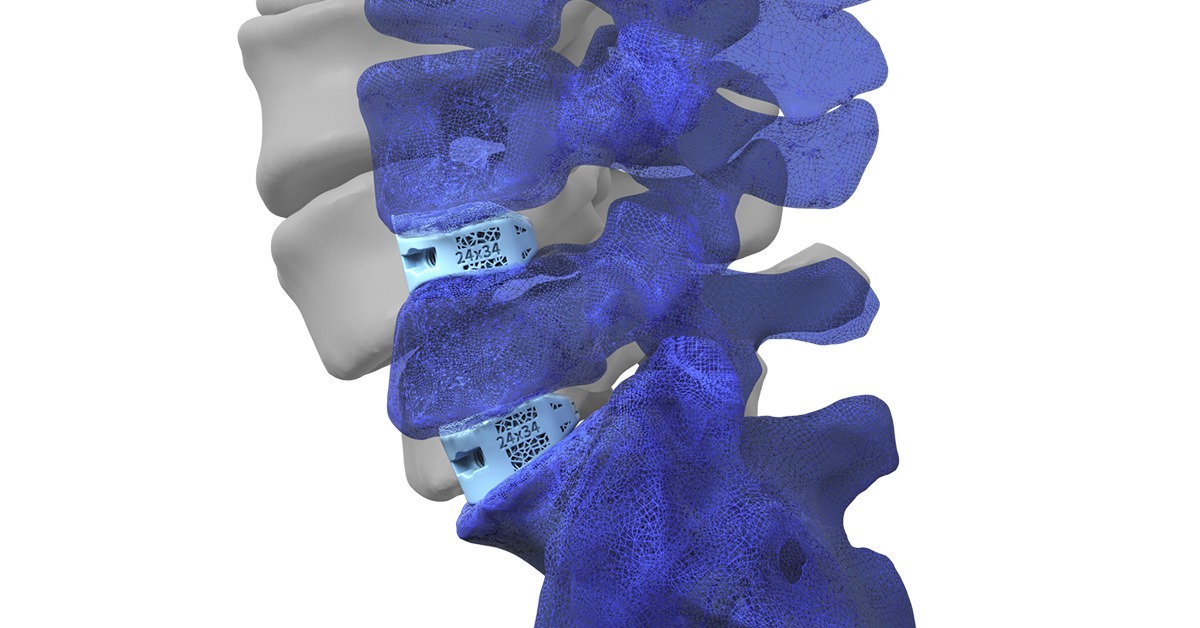
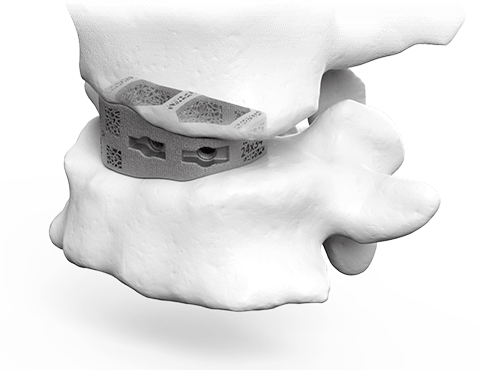
Improved Graft Contact:
94% average aprevo® device to vertebral endplate contact at 1-year follow-up on CT2

Subsidence Mitigation:
96% of personalized aprevo® levels with zero subsidence at 1-year follow-up on CT2

Improved Alignment Restoration in Degenerative Cases:
44% increase in alignment restoration of preoperatively malaligned patients3

Improved Alignment in Complex Adult Deformity:
45% improvement in achieving targeted PI-LL within 5º compared to stock implants4

Reduced Rate of Revisions:
<2% rate of revision surgery for mechanical complications in adult spinal deformity patients from the multi-center COMPASS™ Registry5
Biomechanical studies have shown that endplate matched implants provide:
• 28% decrease in posterior rod stress6
• 50x increase in contact area7
• 30% reduction in stress concentration on the endplate7
aprevo® Implant Registry with 2-year Data
References:
- Sadrameli SS, Blaskiewicz DJ, Asghar J, et al. Predictability in achieving target intervertebral lordosis using personalized interbody implants. Int J Spine Surg. 2024;18(S1):S16-S23. doi:10.14444/8637
- Ames C, Smith J, Nicolau R. Tomographic assessment of fusion rate, implant-endplate contact area, subsidence, and alignment with lumbar personalized interbody implants at one-year follow-up. Intl J of Spine Surg. 2024; 18(S1):S41-S49. doi:10.14444/8640
- Asghar J, Patel AI, Osorio JA, et al. Mismatch between pelvic incidence and lumbar lordosis after personalized interbody fusion: The importance of preoperative planning and alignment in degenerative spine diseases. Int J Spine Surg. 2024;18(S1):S24-S31. doi:10.14444/8638
- Smith JS, Mundis GM, Osorio JA, et al. Analysis of personalized interbody implants in the surgical treatment of adult spinal deformity. Global Spine J. doi:10.1177/21925682231216926
- Kent RS, Ames CP, Asghar J, et al. Radiographic alignment in deformity patients treated with personalized interbody devices: early experience from the COMPASS registry. Int J Spine Surg. 2024;18(S1):S6-S15. doi:10.14444/8636
- Patel R. Does patient-specific implant design reduce subsidence risk in lumbar interbody fusion? A bottom-up analysis of methods to reduce vertebral endplate stress. University of Colorado Denver, 2018.
- Chatham LS, Patel VV, Yakacki CM, Dana Carpenter R. Interbody spacer material properties and design conformity for reducing subsidence during lumbar interbody fusion. J Biomech Eng. 2017;139)5_:0510051-0510058. doi:10.1115/1.4036312

